Watch MUSC: Benign Paroxysmal Positional Vertigo (BPPV)
Certified vestibular therapist, Abeed Hirji, reviews a 5-minute non-invasive office procedure for the treatment of BPPV.
Really, a quick fix? Yes, is my response to this question by many of my patients who come to me whom I suspect may have Benign Paroxysmal Positional Vertigo (BPPV). With a quick 5-minute non-invasive office procedure, we are usually able to treat BPPV with outstanding results!
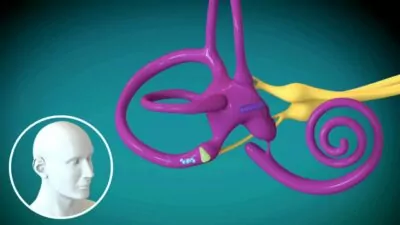
Our patients often come to us having found repetitive ‘lay down – sit up’ exercises on the Internet in an attempt to manage their Benign Paroxysmal Positional Vertigo (BPPV). These approaches, often referred to as Brandt-Daroff exercises, go back to the days when the only treatment for BPPV was thought to be simply trying to habituate to the presence of the otoconia (calcium carbonate crystals) in the semi-circular canal(s). Fortunately, in recent years, it has become recognized that the otoconia can actually be guided out of the affected canal via Canalith Repositioning Maneuvers. The efficacy of this approach is outstanding with 74.8% resolution after one treatment, 93.8% after two treatments, and 98.4% if three treatments are required (Macias et al 2000); and it is much easier on patients than trying to habituate!
This treatment has been studied extensively, and all studies show similar levels of efficacy. Many Doctors are familiar with the Epley Maneuver, which is one Canalith Repositioning Maneuver used to treat the most common presentation of BPPV. However, there are actually twelve different presentations of BPPV with ten different patterns of nystagmus and a minimum of ten different treatment maneuvers required to manage all the variants. All of these variants have distinctly different patterns of positional nystagmus which allows us to:
- Determine if BPPV appears to be the correct diagnosis
- Identify which is the affected canal
- Establish whether it is a Canalithiasis (free-floating otoconia) or Cupulolithiasis (otoconia adhered to the sensory hair bundle or cupula)
These details direct us in knowing the correct maneuver to perform following the appropriate safety screening. Performing the correct maneuver allows a greater chance of success and improved outcomes on immediate repositioning and also helps to prevent the calcium carbonate crystals from displacing into other or multiple canals.
Appropriate post-maneuver protocols (specific to the individual patient) may also be employed by the treating therapist. Any additional advice on preventative measures should also be conveyed to the patient, be it on the initial assessment/treatment day or during future follow-up visits with the therapist. It will be prudent for the therapist to also check for any residual motion sensitivity or imbalance issues that may prevail following successful treatment of BPPV with repositioning maneuvers.
About the Repositioning Maneuvers
Depending on the affected inner ear canal (posterior, anterior, or horizontal), the type of BPPV (canalithiasis or cupulothiasis) and the side (right or left), appropriate maneuvers should be performed to help facilitate canalith (inner ear crystal) migration from the affected semicircular canal to the otolith chamber. Essentially, the ear rocks or crystals are homeless and with the appropriate maneuver employed, the clinician is trying to help them find their home – the otolithic chamber. Repositioning maneuvers consist of head and body movements skillfully performed by the treating clinician, usually performed on an examination table or plinth, and guided by infrared video technology to observe for canal-specific nystagmus and vertigo. The Hallpike and Roll tests are the two common assessment positions used to determine the specific BPPV variant which allows the treating clinician to perform the correct repositioning maneuver. As mentioned, there are various repositioning maneuvers including the particle or canalith repositioning maneuver (i.e. Epley Maneuver), Semont or Liberatory Maneuver, Gufani Maneuver, Appiani Maneuver, Foster Maneuver, Kim Maneuver, BBQ Roll Maneuver, etc. Patients normally feel a little anxious with assuming the Hallpike or Roll test assessment positions as they will usually provoke the patients’ sensation of vertigo which, in many cases, they have been trying to avoid. Repositioning maneuvers may also provoke these same symptoms. As such, the treating clinician must thoroughly explain to the patients what they may expect from the repositioning maneuver and work with the patients to help them through their symptoms. Employing a careful, rush-free, eye-to-eye, heart-centric approach usually helps to ease the patient’s anxiety, which can provide for a more tolerable and maybe pleasurable repositioning experience.
 Of note, patients with post-traumatic BPPV usually require multiple treatments and may experience more frequent recurrences compared to those patients whose BPPV is of idiopathic origin. The theory behind this is that the trauma may have damaged the inner ear organ or altered the blood flow to it, thus affecting the integrity and the malleability of the tissues. Other presumptions suggest that the trauma may damage the actual otoconia (ear crystals), making it difficult for them to move through the semicircular canals.
Of note, patients with post-traumatic BPPV usually require multiple treatments and may experience more frequent recurrences compared to those patients whose BPPV is of idiopathic origin. The theory behind this is that the trauma may have damaged the inner ear organ or altered the blood flow to it, thus affecting the integrity and the malleability of the tissues. Other presumptions suggest that the trauma may damage the actual otoconia (ear crystals), making it difficult for them to move through the semicircular canals.
Prevention of BPPV
It has been theorized that not sleeping on the affected side, performing Brandt-Daroff exercises, and vitamin D supplementation (if low on vitamin D) may help to prevent future or frequent recurrences of BPPV.
By Abeed Hirji, BScOT, BScKIN
Certified Vestibular Rehabilitation Therapist
 Abeed graduated from both Simon Fraser University and the University of British Columbia in 2004, with a Bachelor of Kinesiology and a Bachelor of Occupational Therapy degree, respectively. Since graduation, Abeed has honed his skills in the assessment and treatment of patients with concussions and other forms of traumatic brain injuries. His passion for treating patients with dizziness, vertigo and balance disorders motivated him to seek further education in Vestibular Rehabilitation. To this effort, Abeed achieved his Competency Certification (Advanced) in Vestibular Rehabilitation from Emory University School of Medicine in Atlanta, GA and Duke University School of Medicine in Durham, NC. Abeed is also trained in delivering training on the BrainPort® Balance device.
Abeed graduated from both Simon Fraser University and the University of British Columbia in 2004, with a Bachelor of Kinesiology and a Bachelor of Occupational Therapy degree, respectively. Since graduation, Abeed has honed his skills in the assessment and treatment of patients with concussions and other forms of traumatic brain injuries. His passion for treating patients with dizziness, vertigo and balance disorders motivated him to seek further education in Vestibular Rehabilitation. To this effort, Abeed achieved his Competency Certification (Advanced) in Vestibular Rehabilitation from Emory University School of Medicine in Atlanta, GA and Duke University School of Medicine in Durham, NC. Abeed is also trained in delivering training on the BrainPort® Balance device. 