When Dizziness Affects the Mind
Vestibular disorders are widely recognized for causing dizziness, vertigo, and imbalance. But what many people don’t realize is that these disorders can also significantly affect the brain—particularly in the areas of thinking, memory, and attention. For people with chronic vestibular dysfunction, “brain fog” is more than just a vague feeling. It can interfere with daily life, work, and emotional well-being.
Recent scientific studies have revealed strong links between the vestibular system and cognitive health. Researchers are especially interested in how vestibular loss may contribute to long-term cognitive decline and even dementia. Although the full picture is still emerging, what we do know highlights the need for greater awareness, earlier diagnosis, and more research.
What Is the Vestibular System?
The vestibular system, situated in the inner ear and brain, plays a crucial role in controlling balance, posture, and spatial orientation. It constantly sends signals about motion and head position to the brain, allowing you to walk, turn, and move without losing your balance.
When this system is dysfunctional, as in vestibular neuritis, Meniere’s disease, vestibular migraine, or bilateral vestibulopathy, it can lead to persistent dizziness, motion sensitivity, visual disturbances, and difficulty walking. Less visibly, it can also challenge your brain’s ability to process information.
Why Balance Sensors Affect the Brain
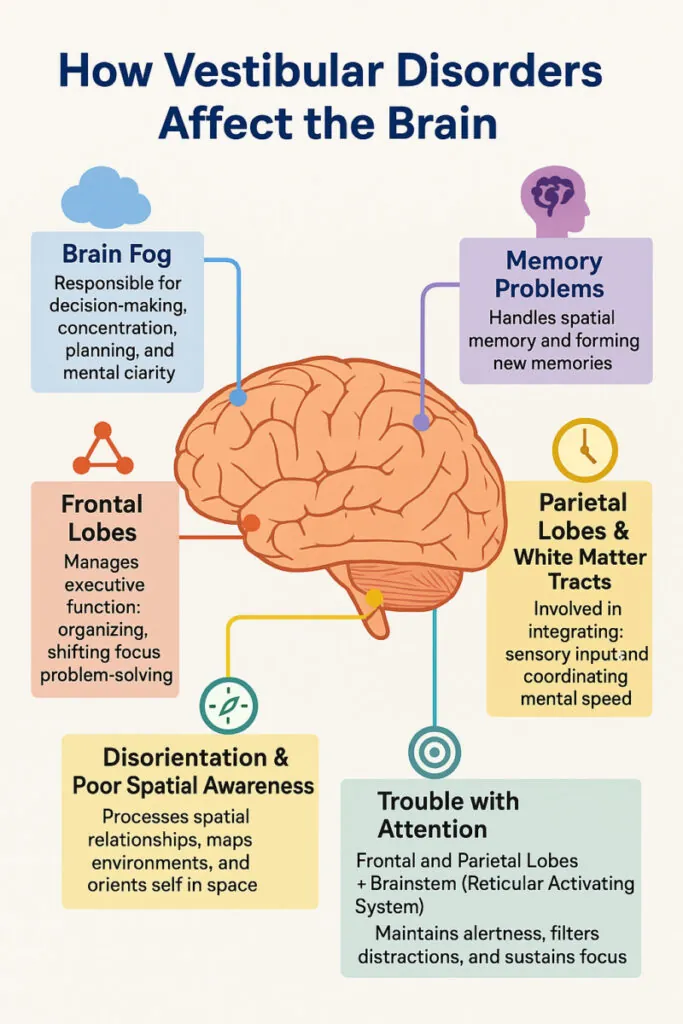
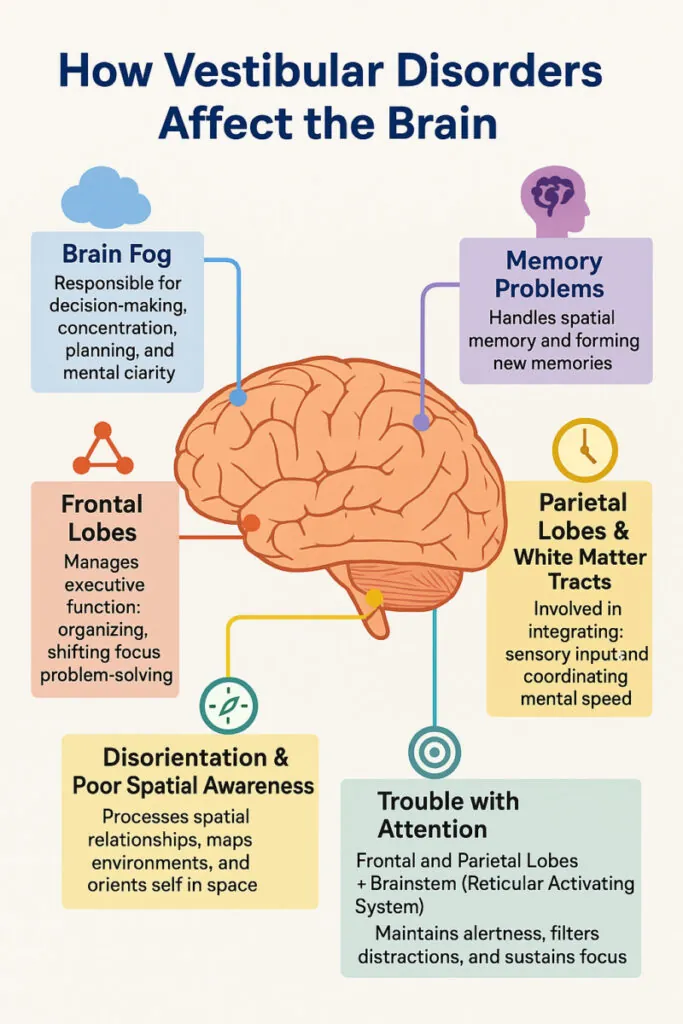
The brain and vestibular system work as a team. The inner ear’s signals are processed by areas of the brain involved in attention, memory, and spatial reasoning—especially the hippocampus (critical for memory) and the prefrontal cortex (important for decision-making and focus).
When vestibular input is disrupted, the brain has to work harder to compensate. This can leave fewer cognitive resources for other tasks like conversation, multitasking, or learning new things. People with vestibular disorders often describe this as “mental fatigue” or “cognitive overload.”
Impact all Life Stages
Vestibular disorders can significantly impact cognitive functioning across all ages, though the effects often differ by life stage. In children, vestibular dysfunction may lead to difficulties with reading, writing, and visual tracking, as well as problems maintaining focus in a busy classroom environment. Poor balance and coordination can also make it harder to participate in sports or play, affecting both physical development and self-esteem. In working adults, the cognitive burden of a vestibular disorder often shows up as trouble multitasking, mental fatigue after meetings or screen time, slower information processing, and difficulty concentrating in visually stimulating or fast-paced environments. These challenges can interfere with job performance and increase stress, especially when cognitive symptoms are misunderstood or overlooked.
 What the Research Shows
What the Research Shows
Numerous studies have confirmed that vestibular dysfunction is associated with cognitive problems:
- A 2016 study in Neurobiology of Aging found that older adults with vestibular loss had reduced volume in the hippocampus, a brain region essential for memory and spatial navigation.
- A 2019 paper in JAMA Otolaryngology reported that vestibular impairment in older adults was associated with poorer performance on memory tests and an increased risk of cognitive decline.
- A 2021 review in Frontiers in Neurology concluded that cognitive deficits—especially in memory, attention, and processing speed—are common in people with chronic vestibular disorders.
- A 2023 paper in Current Opinions in Neurology concluded that vestibular migraine may involve multisensory processes critical for motion perception, spatial orientation, visuospatial attention, and spatial awareness.
In children and adults alike, problems with attention and memory often coincide with vestibular symptoms. Tasks that involve navigating space (like reading a map, remembering directions, or judging distances) are especially difficult.
Vestibular Loss and Dementia Risk
The link between vestibular dysfunction and dementia is one of the most concerning areas of research—and one of the least understood. Several studies have found that people with vestibular loss may be more likely to develop cognitive impairment, including Alzheimer’s disease.
For example:
- A 2017 study published in Geriatrics & Gerontology International found that older adults with dizziness were more likely to show signs of cognitive impairment.
- A 2019 study in Alzheimer’s & Dementia revealed that individuals with vestibular dysfunction had a greater likelihood of developing dementia, even after controlling for age and other health conditions.
Researchers hypothesize that vestibular dysfunction may accelerate brain aging, reduce hippocampal stimulation, or increase the brain’s vulnerability to neurodegenerative disease.
However, these findings are linked but not proven to causation—they show an association, but not a direct cause-and-effect relationship. It’s unclear whether vestibular loss causes dementia, contributes to its progression, or simply occurs alongside other age-related brain changes.
What Researchers Still Don’t Know
Despite growing evidence of the vestibular-cognition connection, there are important gaps in our understanding:
- Causal links are unclear. We don’t yet know whether vestibular dysfunction directly causes cognitive decline, or if both stem from shared risk factors like aging, inflammation, or vascular disease.
- Not all patients experience cognitive issues. It’s still unknown why some people with vestibular disorders develop brain fog or memory problems while others do not.
- Treatment effects on cognition are understudied. While vestibular rehabilitation therapy (VRT) improves physical symptoms, its impact on cognitive function hasn’t been rigorously measured in large-scale trials.
- Long-term studies are lacking. Most current research follows participants for short periods. More long-term, population-based studies are needed to determine whether managing vestibular disorders can help prevent dementia or slow cognitive decline.
Signs You May Be Experiencing Cognitive Effects from a Vestibular Disorder
- Trouble concentrating in noisy or busy environments
- Feeling “foggy” or mentally tired after visual tasks
- Difficulty finding words or remembering conversations
- Trouble reading maps or navigating familiar areas
Managing the Cognitive Load
Even with these gaps, there are practical steps people can take. Vestibular rehabilitation, occupational therapy, and cognitive training may help improve both physical and mental functioning. Strategies such as pacing activities, reducing visual clutter, and taking regular breaks can ease cognitive strain.
It’s also important for healthcare providers to validate and address cognitive symptoms. Too often, “brain fog” is dismissed as anxiety or aging. Recognizing it as a legitimate part of vestibular dysfunction is key to holistic care.
Final Thoughts
The science is clear: vestibular disorders don’t just affect your balance—they can affect your brain. From mild forgetfulness to significant cognitive decline, the mental effects are tangible, measurable, and deeply impactful.
Researchers are still uncovering the full story, particularly regarding the risk of dementia. However, what we already know underscores the need for early detection, patient-centered care, and increased public awareness. If you or someone you love is dealing with both dizziness and mental fog, you are not imagining it, and you are not alone.
As we learn more about the brain-body connection, one message stands out: maintaining vestibular health may be just as important for the mind as it is for the body.
By The Vestibular Disorders Association, Reviewed by Amir Kheradmand, MD, Kristen Steenerson, MD, and Habib Rizk, MD, MSc
 What the Research Shows
What the Research Shows