Medical practices have significantly increased the implementation of patient-centered medical home (PCMH) practices over time to try and provide better care for patients with chronic illnesses, according to an article published online January 5 in Health Affairs.
James A. Wiley, PhD, from the Institute for Health Policy Studies, University of California, San Francisco, and colleagues analyzed data from three national surveys of physician practices conducted between 2006 and 2013.
The trend of implementing PCMH processes overall covers small and medium-size practices, as well as large practices, but large practices have used fewer than half of the recommended processes, they write.
“People with chronic illnesses cost the health care system $1.5 trillion, or about 75 percent of total health care expenditures,” the analysts write.
“Caring for people with chronic illnesses provides a crucial test for health care reform.”
The analysts extracted data from the National Study of Physician Organizations 3, conducted between January 2012 and November 2013; the National Study of Physician Organizations 2, conducted between July 2006 and March 2007; and the National Study of Small and Medium-sized Physician Practices, conducted between July 2007 and March 2009.
Although some incentives existed during the earlier surveys for practices to expand services for chronic care, incentives provided through the Affordable Care Act and the Technology for Economic and Clinical Health apply to the latest survey.
The survey contained questions on care coordination or integration, quality and safety of care, and enhanced access to care. Practices surveyed could be owned by a hospital or health system, by physicians, or by community health center or other owner, but not by academic or government centers. Practices could also be a mixture of primary care physicians and multiple specialties.
The analysts focused on four chronic illnesses: asthma, congestive heart failure, depression, and diabetes.
Progress in Electronic Records
Overall, practices expanded the most in terms of using electronic medical records for progress notes, coordination with the pharmacy, measuring care quality, clinical decision support, and allowing patients online access to their records.
Small to medium-size practices also significantly increased adoption of using nurse managers for care of patients with chronic illness and nonphysician staff for patient education. However, this group declined in having electronic access to emergency department and hospital discharge records and group visits for patients.
Large practices worked more toward participating in care quality improvement collaboratives and the use of plan-do-study-act cycles, but this group declined in providing care feedback to physicians, using patient reminders, and communicating by email with patients.
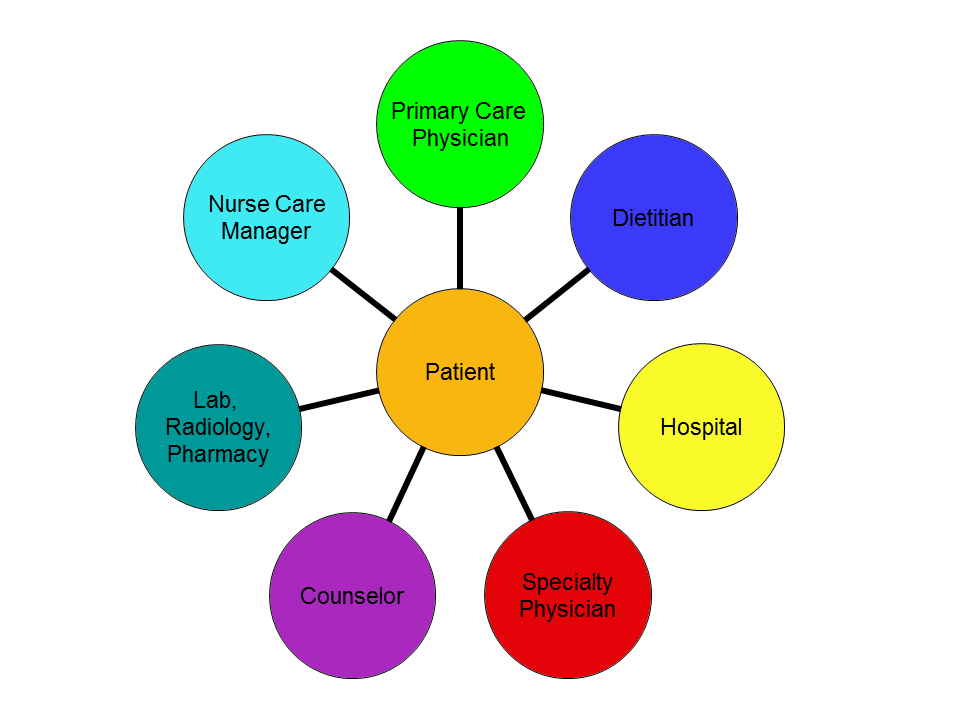
The analysts note that room exists for improvement to several elements of PCMH processes, including use of nurse care managers, registries, and patient communication and access.
“It is particularly sobering to note that even among large practices, fewer than half of the recommended processes are being used, on average,” the analysts write. “Among small practices, the share is less than 30 percent.”
They point out several options, particularly for small practices, for implementing care management processes, including:
- joining larger practices,
- joining hospitals or large multispecialty groups,
- expanding participation in independent practice associations,
- joining an accountable care organization, and
- forming a virtual network to build up to the scale needed.
They conclude, “A major unanswered question is whether or not the steady increase in the capabilities of physician practices to manage patients with chronic illnesses will continue.”
Source: Medscape Medical News, accessed January 9, 2015
