The Vestibular traumatic brain injury (tbi) Connection
What Happens to the Brain and Vestibular System after a Traumatic Brain Injury?
A traumatic brain injury can occur under the following conditions:
- The head strikes a stationary object. Common examples include a fall where the head hits the ground or an object, or hitting the head on an object during an auto accident.
- An object hits the head, such as a ball or stick during sports, or as a result of human collision.
- A quick acceleration/deceleration of the head with no contact to any surface. This can occur in dancers and gymnasts due to rapid movement, or during an auto accident where there appears to be no head trauma. For example, whiplash injuries often occur during motor vehicle accidents and cause a concussion.
These events all cause quick deceleration of the head and shifting of delicate brain tissue inside the skull. Rarely does an accident of this nature occur in a true head-on or forward/backward direction. There is typically a rotational force, as would occur if one were struck on the right or left side of the forehead. If the body is traveling forward or facing forward in a still position and a force occurs off center, the brain sustains a rotational shear force, which causes more trauma to brain structures than only linear forces and therefore can result in a more severe TBI. Loss of consciousness and nausea at the time of injury are signs that rotational forces have occurred and can lead to prolonged recovery from injury.
Current research on athletes shows that nerve signals in the brain are disrupted for 30 days after a single concussion. During this time people are more likely to have another injury if engaged in sport activities. This is because reaction time and brain processing are not normal. We are less likely to see something, like a ball, coming toward the head during this vulnerable period. If more than one concussion occurs, the symptoms are typically worse and recovery time is increased.
Trauma to the brain can result in abnormal vestibular system functioning, and the brain can receive abnormal signals regarding the position and movement of the head in space. When vestibular information is inaccurate, the brain most often relies on visual input to stabilize the head on the body. This means that the visual system becomes the most reliable system to quickly assess one’s position in space and to remain balanced. Relying upon vision alone as the primary source of balance often leads to fatigue and difficulty performing routine daily activities. It is also not uncommon for a concussed brain to overly rely on input from your feet immediately after a TBI, making walking on uneven surfaces or soft surfaces more of a challenge. This can result in excessive energy expenditure to stand and walk, increasing fatigue.
Over-reliance on the visual system for balance can result in eyestrain and tension headaches. If the vestibular system is delivering inaccurate information to the brain about the head’s position in space, the brain must rely on visual input and joint sensors (proprioception) to feel the body in space. Failure to effectively compensate with the use of visual references and being aware of the surface on which one is sitting or standing results in dizziness and a sense of instability. Dizziness encourages a person to refrain from moving the head and leads to neck stiffness and headaches, which can further worsen the severity of the dizziness. The presence of a whiplash associated with the concussion further complicates the diagnosis and limits the ability to participate in life activities. Long-term over-reliance on vision for balance and spatial perception can also cause the brain to become visually dependent, meaning the concussed brain may continue to prioritize information from the eyes above vestibular input, making activities with the eyes closed or in low light more challenging and potentially provoke symptoms.
How Do I Know If I’ve Had a TBI?
There is currently no single diagnostic test for the presence of a concussion. If there is any suspicion of a concussion during sporting activity, an athlete or child should be removed from play to watch and assess their behavior, and in many states medical clearance is necessary to legally return to play. If a person develops signs of neurological injury, such as repeated vomiting, seizures, loss of consciousness, unequal pupil size, confusion, or slurred speech, immediate medical attention is necessary to rule out serious brain trauma. Apart from sports, any mechanism of trauma to the head and neck can result in concussion and should be evaluated if symptoms are present.
Concussion injury does not appear on any routine brain scan such as CT or MRI, and there is no singular diagnostic test for concussions. A diagnosis of concussion is made based on a group of symptoms that can become immediately present or may arise over weeks to months after the injury. Acute symptoms can be present for seven to ten days following the concussion, and the most common recommendation is to limit activities and rest the brain with the anticipation of natural recovery within the first ten days post-concussion. After ten days, it can be safe and beneficial to begin rehabilitation in a conservative and graded manner, beginning with light, non-contact exercise.
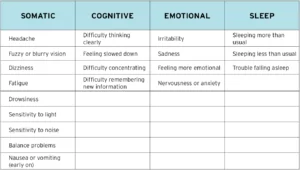
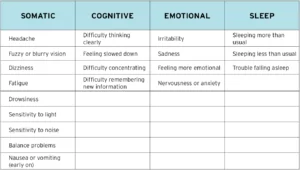
Concussion symptoms typically fall into four categories: physical, emotional, cognitive, and sleep. People who experience a concussion often have one or more symptoms from one or more of these categories.
Why Do Some People Have Few to No Symptoms, Some People Slowly Develop Symptoms Over Time, and Others Feel They Cannot Function Immediately After a TBI?
It can be normal to have no symptoms after a concussive event. In studies of athletes, almost all subjects are free of all symptoms by three days after injury, while brain studies still show reduced nerve signal transmission and risk of injury for up to 30 days. Other people feel normal for two to three weeks, then have a steady increase in headaches, dizziness, or fatigue that at times are not recognized as being caused by the concussion. Men are more likely to lose consciousness and seek out immediate medical care, leading to a lower rate of undiagnosed concussions. Fewer people have immediate and more severe concussive symptoms that last for prolonged time frames. Some risk factors that may lead to prolonged recovery and a greater odds of post-concussive syndrome are prior history of head injury and a history of migraines. Females are at higher risk of developing post-concussion syndrome than males.
Some responses to concussion can be influenced by genetics. People who have a history of dementia or Alzheimer’s disease in their family can be more at risk for having a worse response after a concussion. This is because some people have proteins (Tau) in the brain that already place them at risk of memory problems, which can be aggravated by concussion. This results in more cognitive difficulties with memory, concentration, and motivation after experiencing a concussion.
Due to the forces involved in concussion, it is very common to sustain a whiplash injury that is often not diagnosed with the concussion. As the head decelerates or receives the force of an incoming object, the neck muscles are strained. The effects of whiplash injury are not always immediate and can appear two to three weeks later with an increasing number of tension headaches and visual disturbances. Dizziness can also occur related to neck strain, known as cervicogenic dizziness. This delayed increase in symptoms can interfere with school and work performance.
Many people have previous conditions that make the brain’s response to concussion more problematic. A prior history of migraine headaches can worsen migraines or lead to post-concussive headaches after sustaining a concussion. At times, migraines can occur without headache and produce only an aura that feels like vertigo or dizziness lasting for multiple hours or days. This is thought to be due to the migraines occurring through vestibular processing areas in the brain. Failure to recognize and treat migraine activity can lead to prolonged symptoms and places more stress on the brain, limiting recovery. This is more prevalent in females than males.
A history of visual disturbances or childhood sensory processing issues also affects one’s response to concussion. For example, if a person had difficulty with distance vision or depth perception before the injury, the brain adjusted to that problem. After an injury, the way in which the brain compensates for the visual problem may not work as well, and the ability to focus on static objects or following moving objects may cause symptoms of dizziness, as well as head pressure, head fog, and concentration problems. Likewise, if a prior history of sensory integration problems and motion sickness is present, concussion can cause increased difficulty for the brain to process vestibular information.
How Do Symptoms of Concussion Affect Daily Life?
The concussion injury itself is ‘invisible’, as headache, dizziness, head fog, eye strain, and fatigue are rarely perceived by others. Thus, the disruption of the brain’s ability to process sensory input can result in extreme fatigue, anxiety, and emotional instability. In children, this manifests as behavioral outbursts or tantrums. Highly visual activities overwhelm the brain, so crowded environments, such as work, school, stores, and public events, can cause elevation of symptoms or anxiety.
Work and school performance can suffer as concentration and memory are affected. Adjusting visual focus from near and far can cause dizziness and headache. In schools, looking from the desk to PowerPoint presentations or to or boards in front of the classroom is extremely challenging. Children and adults alike report difficulty with memory and concentration, as well as reduced accuracy in work performance. Students have trouble completing homework, and adults arrive home from work with extreme fatigue and a lack of energy to engage in family and household activities.
Overly stimulating environments can provoke symptoms of headache, dizziness, and imbalance, and can cause anxiety and fear. Over time people tend to withdraw from outings and can become depressed from the inability to perform routine daily activities. Crowded places are difficult to navigate because of the movement of people and complex visual background in the observer’s peripheral vision. These visual distractions cause a sense of imbalance and dizziness, often with head pressure, which can lead to panic attacks or avoidance of activity. People may worry that they will develop symptoms in a public space, such as the grocery store, fearing that others will see and misjudge them, further worsening avoidance behavior and self-isolation.
How Can I Best Cope With Symptoms of Concussion?
The best treatment for symptoms of concussion involves an assessment of vestibular function by a physical therapist. A comprehensive vestibular evaluation should include examination of balance activities that involve the vestibular, vision, and proprioceptive systems, which reveals how the brain interprets movement of the body and head relative to space and the visual surroundings. A cervical examination determines if neck sprain or dizziness from the neck is contributing to symptoms and perpetuating headaches. Based on examination findings, customized exercises and recommendations for participating in or modifying school, work, and home activities expedites recovery.
If necessary, medical assessment by a primary care physician or neurologist can help determine if migraine headaches are present and whether medication could improve recovery. Finally, those with ongoing eye-tracking problems that interfere with reading and computer-related tasks benefit from vision examinations, usually performed by optometrists or ophthalmologists who have completed residency programs in vision therapy and rehabilitation. Physical and occupational therapists may also provide vision therapy to improve eye tracking and eye accommodation, meaning the ability to accurately move the eyes from near and far targets.
Following are tips that can help a person reduce symptoms throughout the day. More specific, personalized recommendations are provided during vestibular therapy, and extensive education regarding how the vestibular system works helps one accept and cope with the recovery process.
In the home:
- Limit visual activities to shortened time intervals with frequent rest breaks. Set a kitchen timer to engage in visual activities for 30-45 minutes, then allow for 10-15 minutes to relax the eyes and perform grounding exercises that focus on feeling the body firmly seated in a chair.
- Utilize the 20/20/20 rule, which recommends that you look away from your computer or book every 20 minutes and focus on an object roughly 20 feet away, for 20 seconds.
- Utilize “grounding” techniques when experiencing dizziness or imbalance by sitting in a firm seat with a back and arm rests or lean against a wall to improve spatial awareness via proprioception.
- Use a line guide such as a bookmark or index card when reading to reduce the work involved for the eyes to scan.
- Listen to books on tape when possible to reduce eye fatigue.
- Limit scanning/scrolling on the computer, enlarge fonts, and adjust the screen settings to reduce glare.
- Limit blue spectrum light exposure, such as from digital devices.
- Pace yourself and limit the number of activities you perform per day.
- Do not allow your symptoms to become severe.
- Do not save all your errands for one day, then stay home for 5 days. It is better to do one errand per day to gain some exposure to different environments, then return home to calm symptoms down and feel a sense of success and achievement. Saving all your errands for one day will potentially exhaust you and increase your symptoms so that it can take multiple days to recover.
At school:
- Initially, a student may need to miss one to two weeks of school and may not be able to attend full days of school upon return. Try to keep up with work at home, as getting behind can cause increased anxiety. Work in short intervals of time.
- Extending the time to complete assignments typically induces stress, whereas reducing the volume of the assignment can allow for an understanding of the material without getting too far behind.
- Request copies of presentation material to avoid rapid movement of visual focus from the table to distant targets.
- “Early passing” (i.e. transferring between classes before or after the large bulk of students) can be requested to avoid the visual chaos of people moving through a crowded space.
- A 504 (accommodation) Plan can be established if recovery is prolonged and symptoms are persistently increased throughout the school day, causing a decline in the student’s performance.
At work:
- Avoid working under fluorescent lighting.
- Arrive early to meetings and select a seat that provides the least offensive visual background. Avoid looking directly at linear backgrounds such as vertical or horizontal blinds, or a wall of bookshelves.
- Use lunchtime to settle any symptoms, and avoid noisy or overcrowded gathering places. As you feel better, gradually join the group.
- Utilize the 20/20/20 rule to limit symptoms related to prolonged computer screen exposure (see above).
Socially:
- It is important to maintain contact with peers and friends who are supportive and to remain socially and emotionally engaged.
- Limit social activities to small groups of people for only one to two hours at a time, and gradually lengthen outings as they are well tolerated.
- If eating out, go early or late and request a table on the outer edge of the restaurant and face a wall to avoid seeing servers moving in the background.
- Initially avoid visually stimulating environments such as movies, sporting venues, performing arts venues that have altered lighting, placed with loud noises, and stadium-style seating.
- Think about joining a vestibular disorders support group. You are not alone and others dealing with prolonged concussion symptoms may have helpful advice or insight.
For travel:
- Airports are visually complex, and people do not abide by traffic patterns, causing visual chaos. Arrive early, check-in and find a quiet location near your gate to sit facing a wall or less stimulating visual surround. Allow 10-15 minutes to feel that your body is still in a chair and to calm any dizziness.
- If you become anxious due to symptom onset in busy environments, have a discussion with your physician about anxiety medications.
- While out of town, try to be flexible with your itinerary and schedule periods of rest or seated breaks to allow symptom reduction. Foreign environments are more visually complex for the brain to process, whereas the home environment is relaxing and predictable.
How Can I Prevent Future Injury?
The best way to prevent subsequent concussion is to allow full recovery from any injury before resuming activities that are risky. Full recovery means there are no symptoms with any activity, whether academic, work-related, during leisure activities, or during sports. Use any recommended safety equipment appropriately, ensure all coaches are fully trained in concussion avoidance, identification, and treatment, and know your personal concussion history. Stop participating in sports or leisure activities if there is any indication of potential injury to the head or neck, and seek medical attention.
By Nicole Miranda, PT, DPT, with edits by: John Patrick Dorangricchia, PT, DPT
Additional Resources: