Ear Anatomy
Overview The fluid within the inner ear's membranous labyrinth is called endolymph (endo-: inside or within). The fluid contained between the bony labyrinth and the membranous labyrinth is perilymph (peri-: around or about). These two
Peer Reviewed
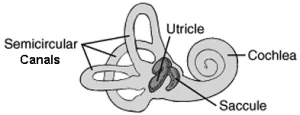
The peripheral vestibular system includes the organs of the inner ear, also known as the labyrinth, which contains two primary structures: the cochlea, responsible for hearing, and the vestibular apparatus, responsible for maintaining balance, stability and spatial orientation. This article examines these in more detail, including: semicircular canals, utricle, saccule, vestibular nerve, oval and round windows, vestibuloocular reflex, vestibulocollic reflex, and vestibulospinal reflex.
There are two components of the vestibular system: the central system (brain and brainstem) and the peripheral system (inner ear and nerves to brainstem). The inner ear has two primary components: the cochlea and the vestibular apparatus (semicircular canals, utricle, and saccule). The cochlea is responsible for hearing and the vestibular apparatus is responsible for balance and position.

Figure 1

These structures are housed within a hollowed cavity of the human skull known as the bony labyrinth. The bony labyrinth contains a fluid called perilymph (peri-: around or about). Suspended in perilymph is another set of ducts and chambers called the membranous labyrinth. The membranous labyrinth is filled with endolymph (endo-: inside or within). This system can be thought of as a tube within a tube.
The two fluids contain similar chemicals including sodium and potassium, but their compositions are very different. If the composition of either fluid is disturbed, as in the case of Ménière disease, patients may experience vestibular symptoms (dizziness, vertigo, imbalance) or other ear symptoms (ringing/humming, fullness, hearing loss).
The vestibular apparatus is the most outer part of the peripheral vestibular system. It consists of three semicircular ducts responsible for detecting rotational movement of the head and the otolithic organs (utricle and saccule) that detect linear motion of the head.
The semicircular ducts are a part of the membranous labyrinth within the bony semicircular canals that detect the rotational movement of the head about the axes of motion (X, Y, and Z). There are three semicircular ducts: superior, lateral, and posterior. Each semicircular duct detects the motion of the head around a different axis. The superior semicircular duct detects rotational movement around the frontal, or X, axis (e.g. nodding your head to indicate “yes”). The lateral semicircular duct detects movement around the vertical, or Y, axis (e.g. shaking of the head to indicate “no”). The posterior  semicircular duct detects movement around the anterior-posterior, or Z, axis (e.g. touching your ear to your shoulder).
semicircular duct detects movement around the anterior-posterior, or Z, axis (e.g. touching your ear to your shoulder).
Located at the base of each semicircular duct is a widened area called the ampulla. The ampulla contains the cupula and hair cells. The cupula is a gelatinous structure that spans the entire duct, and its motion is coupled to the hair cells. The hair cells are receptor cells that have hairlike projections called hair bundles that extend into the cupula. When the head moves, the endolymph lags behind due to inertia, which creates a fluid wave that collides with the cupula. The deflection of the cupula, and the hair bundles, activates the hair cells, sending a signal to the brainstem via the vestibular nerve, a branch of the vestibulocochlear nerve. This is how the semicircular ducts detect and transmit rotational movement information to the central nervous system to maintain balance and position. In addition, this information is used by our brain to carry out corresponding eye movements as our head turns to maintain forward vision. Each ear has a matching set of semicircular ducts and canals, and they work in tandem. Vestibular symptoms may be seen in semicircular duct disturbances such as benign paroxysmal positional vertigo (BPPV), superior canal dehiscence syndrome (SCDS), and alcohol positional nystagmus.
 The utricle and the saccule are involved with the linear motion of the head. These two membranous structures, referred to as the otolithic organs, are the sole residents of the vestibule, a hollow cavity located between the cochlea and the semicircular canals. The utricle detects linear motion in the horizontal plane (e.g. accelerating/decelerating in a car) and the saccule detects linear motion in the vertical plane (e.g. movement in an elevator).
The utricle and the saccule are involved with the linear motion of the head. These two membranous structures, referred to as the otolithic organs, are the sole residents of the vestibule, a hollow cavity located between the cochlea and the semicircular canals. The utricle detects linear motion in the horizontal plane (e.g. accelerating/decelerating in a car) and the saccule detects linear motion in the vertical plane (e.g. movement in an elevator).
The otolithic organs each contain a single curved structure called the macula that contains receptor cells known as hair cells and additional supporting cells. Like the mechanism of the semicircular ducts, these hair cells contain tiny hairlike projections. These projections extend into a gelatinous membrane called the otolithic membrane. Resting on top of this membrane are microscopic crystals made of calcium carbonate called otoconia. These are commonly referred to as “ear rocks” or “ear stones.” Upon linear motions of the head, these tiny crystals will drag along the otolithic membrane and deflect the hairlike projections of the hair cell. This deflection allows the hair cells of the otolithic membranes to fire off a signal to the vestibular nerve and communicate with the brain that the head is moving in the horizontal and/or vertical plane.
Dysfunctions of the otolithic organs may lead to vestibular disorders such as BPPV. It can also cause symptoms of brain fog and imbalance. It is not uncommon to have a dysfunction of those organs (or of their central pathways) in vestibular migraine patients.
The information of the inner ear is relayed to the brainstem via the vestibulocochlear nerve which is the eighth cranial nerve (CN VIII). This nerve is considered part of the peripheral vestibular system until it enters the brainstem. The vestibulocochlear nerve is formed by the vestibular nerve and the cochlear nerve after they leave the inner ear. The vestibular nerve is divided into a superior and inferior portion. The superior vestibular nerve relays information from the  anterior semicircular canal, horizontal semicircular canal, saccule, and part of the utricle. The inferior vestibular nerve serves the posterior semicircular canal and most of the utricle. Vestibular disorders may involve one portion of the vestibular nerve or both. Vestibular neuritis most commonly affects both portions but is more likely to affect the superior vestibular nerve when only one is involved. When the superior branch is affected, it is not uncommon for patients to develop BPPV a few weeks after their vestibular neuronitis presentation.
anterior semicircular canal, horizontal semicircular canal, saccule, and part of the utricle. The inferior vestibular nerve serves the posterior semicircular canal and most of the utricle. Vestibular disorders may involve one portion of the vestibular nerve or both. Vestibular neuritis most commonly affects both portions but is more likely to affect the superior vestibular nerve when only one is involved. When the superior branch is affected, it is not uncommon for patients to develop BPPV a few weeks after their vestibular neuronitis presentation.
Each ear has a vestibular nerve, and they work together. Disruption of the vestibular nerve can lead to vestibular symptoms such as vertigo, dizziness, and imbalance. These symptoms can last from hours to days until the brain adapts or the nerve heals. Sometimes vestibular rehabilitation may be needed to restore the function of the peripheral vestibular system or adapt the way the brain interprets the information.
The oval window and the round window are separate membranous structures that lie between the inner and middle ear. These two structures are involved in the transmission of sound waves from the middle ear to the inner ear. Both the oval window and round window are potential sources of a perilymphatic fistula. In this condition, fluid from the inner ear leaks into the middle ear, and the disturbance of fluid content and volume can lead to vestibular symptoms.
The vestibular system is responsible for maintaining balance and position. Several involuntary responses (reflexes) maintain these functions by stabilizing the body and vision. These include the vestibular ocular reflex, vestibular colic reflex, and vestibular spinal reflex.
The vestibuloocular reflex (VOR) is a reflex involving the vestibular and visual pathways that stabilizes the eyes during head motions. This is one of the fastest reflexes in the human body as the speed is necessary to maintain clear vision. As the head moves, the eyes move in equal and opposite directions through the VOR. When running and walking, the head is constantly bobbing and swaying yet we can maintain clear and steady vision. Without the VOR, objects may appear to jiggle or vibrate, and this illusion of movement is referred to as oscillopsia.
There are many methods of testing the VOR including the head-impulse test (HIT)/head thrust test. This test may be performed manually or with the assistance of high-speed cameras. When assessed manually, the clinician will thrust the patient’s head in one direction and see if the patient can maintain a steady, forward gaze. In a video head impulse test (vHIT), video goggles are placed on the patient to track eye stabilization during head movements. This method provides quantitative, objective data for the VOR.
See a demonstration of the head thrust test performed by Dr. Habib Rizk here. (Video)
The vestibulocollic reflex (VCR) is the activation of neck musculature in response to vestibular signals which stabilizes the head. The VCR can be evaluated by vestibular evoked myogenic potential (VEMP) testing. VEMP testing involves the stimulation of one ear with a sound click or pulse while simultaneously measuring the activity of neck muscles (cervical VEMP) or eye muscles (ocular VEMP) in response to stimulation. VEMP testing may be used to assist with the diagnosis of superior canal dehiscence syndrome, Ménière’s disease, and vestibular migraine.
The vestibulospinal reflex (VSR) is an interaction between vestibular signals from the inner ear and spinal nerves. This reflex produces skeletal muscle contractions opposite to the vestibular information to stabilize the body and maintain posture. For example, if our torso is pushed forward from behind, the vestibular system relays information to the spine, and back muscles are activated to prevent a forward fall. Without the VSR, humans would have a much greater risk for falls. The VSR can be tested through computerized dynamic posturography.
Summary
In this article, we have reviewed the anatomy of the peripheral vestibular system and its function. There are several complex reflexes controlled by the vestibular system, and the status of these reflexes can assist clinicians with diagnosing or ruling out certain vestibular disorders. For more information on vestibular testing please see the VeDA article, Tests for Diagnosing Vestibular Disorders.
Authors: Brian Keith,1,2 Habib Rizk MD MSc1
Affiliations: 1Department of Otolaryngology – Head and Neck Surgery, Medical University of South Carolina, Charleston, SC, USA, 2School of Osteopathic Medicine, Campbell University, Lillington, NC, USA
Ahmed ZM, Beaudoin KS, Bojrab DI, et al. Clinical Otology. 4th ed. (Pensak ML, Choo DI, eds.). Thieme; 2015. doi:10.1055/b-002-102380
Curthoys IS, Grant JW, Burgess AM, Pastras CJ, Brown DJ, Manzari L. Otolithic Receptor Mechanisms for Vestibular-Evoked Myogenic Potentials: A Review. Front Neurol. 2018;9:366. Published 2018 May 25. doi:10.3389/fneur.2018.00366
Moini J, Piran P. Chapter 12 – Auditory system. In: Moini J, Piran P, eds. Functional and Clinical Neuroanatomy. Academic Press; 2020:363-392.
Beh SC. The Neuropsychology of Dizziness and Related Disorders. Otolaryngol Clin North Am. 2021;54(5):989-997. doi:10.1016/j.otc.2021.05.016
Sarna B, Abouzari M, Merna C, Jamshidi S, Saber T, Djalilian HR. Perilymphatic Fistula: A Review of Classification, Etiology, Diagnosis, and Treatment. Front Neurol. 2020;11:1046. Published 2020 Sep 15. doi:10.3389/fneur.2020.01046
Taylor RL, McGarvie LA, Reid N, Young AS, Halmagyi GM, Welgampola MS. Vestibular neuritis affects both superior and inferior vestibular nerves. Neurology. 2016;87(16):1704-1712. doi:10.1212/WNL.0000000000003223
Zaleski-King, A.C., Lai, W., Sweeney, A.D. (2019). Anatomy and Physiology of the Vestibular System. In: Babu, S., Schutt, C., Bojrab, D. (eds) Diagnosis and Treatment of Vestibular Disorders. Springer, Cham. https://doi.org/10.1007/978-3-319-97858-1_1
Kristjansson E, Treleaven J. Sensorimotor function and dizziness in neck pain: implications for assessment and management. J Orthop Sports Phys Ther. 2009;39(5):364-377. doi:10.2519/jospt.2009.2834
Fife TD, Satya-Murti S, Burkard RF, Carey JP. Vestibular evoked myogenic potential testing: Payment policy review for clinicians and payers. Neurol Clin Pract. 2018;8(2):129-134. doi:10.1212/CPJ.0000000000000430
Are you tired of searching for the latest vestibular news? Then sign up for VeDA's free monthly newsletter! V-News includes information on current research, patient stories, VeDA events, and more! It's easy to subscribe, and just as easy to unsubscribe.
Give it a try!